MyEMCert Subscription Available on Med-Challenger FUSE
Complete MyEMCert subscription now available on the new Med-Challenger FUSE LMS. Includes didactic topical review, case-based questions, and built-in...
Recurrent pneumonia + systemic aortic feeder on CT suggests pulmonary sequestration. Definitive treatment is surgical resection; embolization is selective.
Recurrent “pneumonia” in a young adult plus a systemic arterial feeder on CT should trigger pulmonary sequestration and definitive surgical resection.
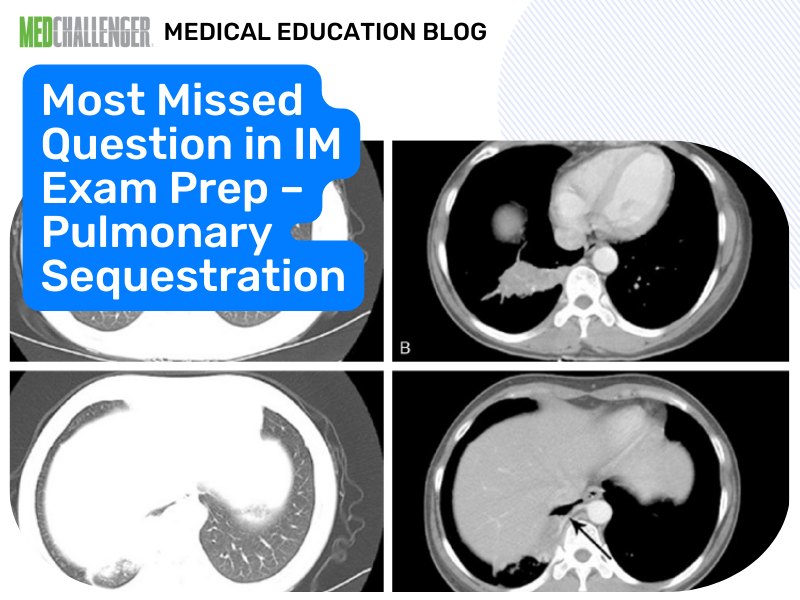
A 26-year-old woman with no previous medical history has experienced 3 episodes of pneumonia in the last year. She has recovered well each time after several courses of oral antibiotics. She is currently hospitalized with her third episode, which was when she presented with fever, cough, and hemoptysis. Her sputum culture shows normal flora. Her HIV testing is negative. Her level of immunoglobulin G (IgG) total and subclasses are within normal limits. Computed tomography (CT) of the chest is shown in the Figure.
 Figure.
Figure.
The lung and mediastinal window show a mass (see Panels A-C). Panel D shows a vessel coming from the abdominal aorta into the mass.
What treatment would you suggest?
Validated correct answer: C. lobar resection. This aligns with contemporary thoracic surgery consensus and standard practice references: pulmonary sequestration (especially symptomatic intralobar sequestration with recurrent infections/hemoptysis) is treated definitively with surgical resection (segmentectomy or lobectomy based on anatomy). Endovascular embolization can be used in select scenarios (e.g., preoperative reduction of blood flow, high surgical risk), but is generally not considered the most definitive therapy due to risks of incomplete occlusion and recurrence/revascularization.
Clinicians miss this because they anchor on “recurrent pneumonia = immunodeficiency” or “treat longer with antibiotics,” but the CT finding of a systemic arterial feeder from the aorta is a board-style “red flag” for sequestration—an anatomic problem requiring an anatomic fix.
- Recurrent pneumonia triggers reflex workup for immunodeficiency while overlooking structural lung disease (sequestration, bronchiectasis, obstruction).
- Test-takers underweight the single most diagnostic clue: arterial supply from the abdominal aorta.
- Confusion about whether embolization is “definitive” rather than adjunctive/selected-case therapy.
| Option | What It Tests / Implies | Why It’s Wrong Here |
|---|---|---|
| A. percutaneous embolization | Knowledge of endovascular approaches to systemic feeders | Can be useful adjunct/selected alternative, but **not the most definitive standard** for symptomatic sequestration; recurrence/revascularization can occur. |
| B. prolonged course of antibiotics | Anchoring on infection-only management | Treat acute pneumonia as needed, but **recurrent infections** from sequestration require definitive correction; “prolonged” antibiotics do not address the lesion. |
| C. lobar resection | Definitive management of pulmonary sequestration | **Correct:** symptomatic sequestration with recurrent infection/hemoptysis → surgical resection (segmentectomy/lobectomy depending on extent). |
| D. retesting with higher-generation HIV test | Overemphasis on occult immunodeficiency | HIV and IgG evaluation are reassuring; CT shows **anatomic systemic arterial supply**, which is diagnostic and management-defining. |
A lung mass with a systemic arterial feeder from the aorta + recurrent pneumonias/hemoptysis = pulmonary sequestration → surgical resection.
1. Identify pulmonary sequestration based on recurrent infections/hemoptysis and CT evidence of systemic arterial supply.
2. Select definitive management for symptomatic pulmonary sequestration (typically surgical resection; embolization reserved for select cases/adjunct).
The stem intentionally “clears” immunodeficiency (negative HIV, normal IgG) and then hands you the pathognomonic imaging clue: aberrant systemic arterial supply from the abdominal aorta. Boards reward recognizing when antibiotics are supportive but not definitive—this is a congenital anatomic lesion that requires surgical management.
A 30-year-old with recurrent left lower lobe pneumonias has CT angiography showing an anomalous artery from the descending thoracic aorta supplying a posterior basal lung segment that does not communicate with bronchi. Best next step for definitive management?
A — Review: Antibiotics don’t correct the anatomic lesion causing recurrence.
B — Correct response!: Definitive therapy for symptomatic sequestration is resection (segmentectomy/lobectomy depending on anatomy).
C — Review: Immunodeficiency workup is not the key once systemic arterial supply is demonstrated.
D — Review: Not asthma; doesn’t address systemic arterial sequestration.
E — Review: Observation may be considered in select asymptomatic cases, but recurrent infections favor definitive treatment.
A patient has chronic cough and daily sputum production; HRCT shows diffuse bronchial dilation in multiple lobes without systemic arterial anomaly. Best diagnosis?
A — Review: Sequestration is focal dysplastic lung with systemic arterial supply, not diffuse airway dilation.
B — Correct response!: Diffuse bronchial dilation on HRCT is classic for bronchiectasis. C — Review: PE would not cause diffuse bronchial dilation.
D — Review: Sarcoidosis typically shows hilar adenopathy/interstitial patterns.
E — Review: HP shows ground-glass, mosaic attenuation, centrilobular nodules.
A — Review: Untreated lesions can cause recurrent infection/hemoptysis.
B — Correct response!: In selected high-risk patients, embolization may be used as an alternative/palliative or bridging approach.
C — Review: Not inflammatory lung disease. D — Review: Antibiotic prophylaxis is not a definitive strategy and carries harms.
E — Review: The key vessel is systemic (aortic) supply; bronchial artery embolization alone misses the mechanism.
Which clinical presentation most strongly suggests intralobar sequestration?
A — Review: More suggestive of large congenital pulmonary airway malformation or diaphragmatic issues.
B — Correct response!: Intralobar sequestration often presents later with recurrent infections/hemoptysis, commonly in lower lobes.
C — Review: Suggests asthma.
D — Review: Suggests TB or fungal disease.
E — Review: Not consistent with sequestration.
Which imaging finding is most diagnostic of pulmonary sequestration?
A — Review: Small airway infection/bronchiolitis pattern; not specific.
B — Review: Nonspecific (edema, infection, inflammation).
C — Correct response!: Systemic arterial feeder is the defining feature of sequestration.
D — Review: Asbestos-related disease.
E — Review: Cardiogenic pulmonary edema.
How would your management differ between an asymptomatic incidental sequestration found on imaging versus symptomatic disease with recurrent infections/hemoptysis, and what factors would push you toward embolization versus surgical resection?
Q2: Is embolization ever “correct” on exams?
A: It can be, but usually in a non-surgical candidate or as adjunct/preoperative management; the exam-default “definitive” answer for symptomatic sequestration is resection.
Q3: Why doesn’t “prolonged antibiotics” solve the problem?
A: Because the core issue is nonfunctioning lung tissue with abnormal blood supply and poor drainage, predisposing to repeated infection despite adequate short-course therapy.
Q4: What presentations should make you consider congenital lung lesions in adults?
A: Recurrent infections in the same location, hemoptysis, and imaging showing a focal mass/cystic change—especially with atypical vascular anatomy.
This question appears in Med-Challenger Internal Medicine Review with CME
Try for free and save. Ace your exams and meet your CME/MOC requirements for just $35 a month!
No matter your program, no matter the size, Med-Challenger for Groups and Institutions can better prepare your program or group, fulfill industry requirements, and increase test scores.
Complete MyEMCert subscription now available on the new Med-Challenger FUSE LMS. Includes didactic topical review, case-based questions, and built-in...
Exam tip: For uncomplicated pediatric mastoiditis, start IV beta‑lactam therapy; reserve vancomycin for MRSA risk. Quick boards rationale.
DEA moves to reclassify marijuana, fulfill MOC needs, providers have questions regarding AI and patient care, and nursing program enrollment down
Stay informed of new medical education content, certification requirements and deadlines, case-based CME quizzes, and special offers.