Most Missed Question in Peds Prep — Vascular Lesion vs Cephalohematoma
Exam-focused review: distinguish neonatal vascular lesions, cephalohematoma, and caput — high-yield Peds Prep question.
School-aged atypical CAP needs a macrolide; preschool bacterial CAP uses amoxicillin. Antivirals for severe influenza pneumonia.
Key takeaway: In preschoolers, viral CAP predominates; use amoxicillin for suspected typical bacterial CAP, macrolides for school-aged children with suspected atypical CAP, and give influenza antivirals for moderate–severe suspected influenza.
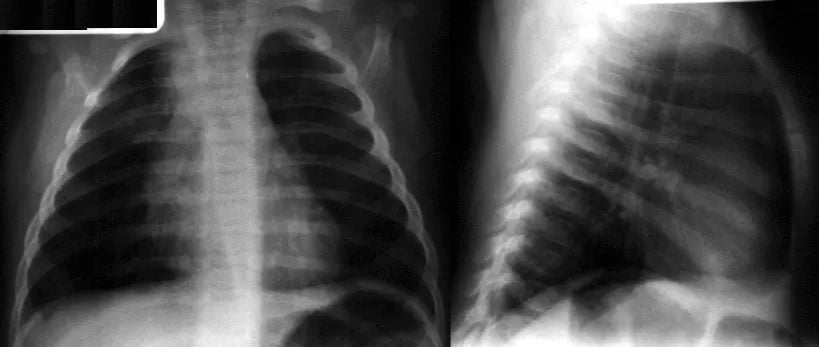
A 3-year-old boy presents with a 1-week history of worsening congestion and cough with persistent fever. His lung examination reveals rales, and a chest radiograph is shown in the figure below.
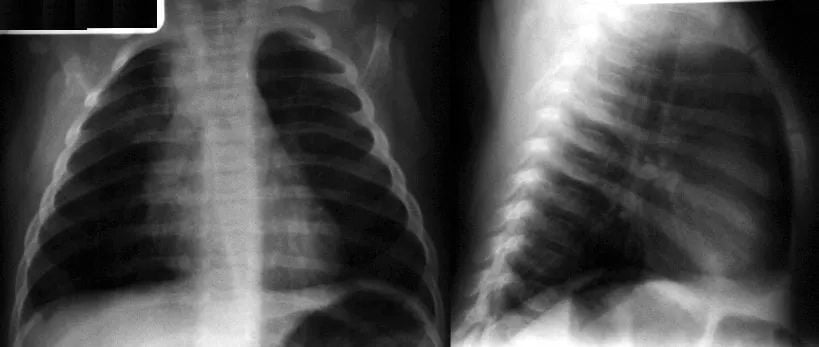
Empiric antibiotic management of community-acquired pneumonia in children is largely based on age and clinical condition. Which of the following statements is true regarding diagnosis and treatment?
Answer Options:
A. The great majority of cases of clinical disease in preschool-aged children can be attributable to bacterial causes.
B. Preschool-aged children with mild community-acquired pneumonia that is thought to be of bacterial origin is usually due to an atypical pathogen.
C. A macrolide should be prescribed for school-aged children with pneumonia due to an atypical bacterial pathogen.
D. Influenza antiviral therapy should be avoided in children with severe symptoms of pneumonia due to possible worsening of the condition.
E. Preschool-aged children do not contract pneumonia from atypical bacterial pathogens.
This item tests age-based CAP epidemiology and treatment selection. Many miss it by over-attributing bacterial causes in preschoolers or by misplacing the role of macrolides. Current guidance emphasizes that preschool CAP is predominantly viral; when bacterial, S. pneumoniae is typical and amoxicillin is first-line. In contrast, school-aged children with a clinical picture suggestive of atypical CAP (subacute onset, dry cough, extrapulmonary features) should receive a macrolide.
The keyed answer is correct. AAP Red Book (2024) and AAFP (2021) reaffirm macrolides for suspected atypical CAP in school-aged children and recommend influenza antivirals for moderate–severe suspected influenza disease even prior to test confirmation (CDC 2024–2025).
Confusion about pathogen prevalence: viral predominance in preschoolers vs atypical pathogens in school-age children.
Overgeneralization of “atypical pneumonia” to all ages; under-recognition that S. pneumoniae remains the typical bacterial pathogen in younger children.
Misconception that influenza antivirals should be withheld until confirmation or due to severity.
| Option | What It Tests / Implies | Why It’s Wrong Here |
|---|---|---|
| A | Etiology in preschool CAP | Viral causes predominate; bacterial is not the “great majority” (AAP 2024, AAFP 2021). |
| B | Atypical pathogens in preschoolers | If bacterial in preschoolers, S. pneumoniae is most common; atypicals are less common. |
| C | Macrolide use for atypical CAP | Correct: school-aged children with suspected atypical CAP should receive a macrolide. |
| D | Antivirals in severe influenza pneumonia | Antivirals should be given for moderate–severe suspected influenza; do not avoid (CDC 2024–2025). |
| E | Absolute exclusion of atypicals in preschoolers | Overly categorical; atypicals can occur but are less common in preschoolers. |
School-aged child with subacute cough and extrapulmonary findings → think Mycoplasma pneumoniae → start a macrolide.
The stem features a preschooler and a CXR, tempting you toward “bacterial CAP = atypical coverage,” but the question asks for a global truth about diagnosis and treatment—most reliable statement is the macrolide recommendation for school-aged atypical CAP.
A 2-year-old with fever, cough, and diffuse wheeze; viral PCR pending; CXR not required. Which is most accurate?
A. Start azithromycin for atypical coverage.
B. Start high-dose amoxicillin routinely.
C. Most preschool CAP is viral; antibiotics often unnecessary if mild.
D. Order procalcitonin to decide on antibiotics.
E. Admit for IV ceftriaxone.
- A — Review: Atypical pathogens are uncommon in preschoolers.
- B — Review: Not all preschool CAP warrants antibiotics; reserve for convincing bacterial features.
- C — Correct response!: Viral etiologies predominate; consider supportive care in mild disease (AAP 2024; AAFP 2021).
- D — Review: Procalcitonin has limited utility in outpatient pediatric CAP decision-making.
- E — Review: No admission criteria met; outpatient supportive care appropriate.
A 3-year-old with high fever, focal crackles, toxic appearance. Best empiric outpatient antibiotic?
A. High-dose amoxicillin
B. Amoxicillin–clavulanate
C. Azithromycin
D. Doxycycline
E. Levofloxacin
- A — Correct response!: Targets S. pneumoniae first line (AAP 2024; BTS 2019).
- B — Review: Consider if beta-lactamase–producing organisms suspected (e.g., concurrent otitis/sinusitis).
- C — Review: Reserve for suspected atypical disease in school-aged children.
-D - Review: Doxycycline (D) isn’t appropriate for a few practical and clinical reasons. It isn’t considered a first-line agent for community-acquired pneumonia in young children, both because beta-lactams provide more reliable coverage of pneumococcus and because doxycycline is generally reserved for older children who might have atypical pathogens. Although brief courses of doxycycline are now considered safe even in younger kids, its role remains limited, and it doesn’t add value over amoxicillin for the pathogen most likely to be causing this child’s illness.
-E - Review: Levofloxacin (E) is avoided unless there is a compelling reason, such as severe allergy to first-line antibiotics or resistant organisms with no safe alternatives. Fluoroquinolones provide unnecessarily broad coverage for an otherwise straightforward pediatric pneumonia, and concerns about adverse effects keep them as a last resort. A stable outpatient three-year-old with presumed pneumococcal disease has no indication for a fluoroquinolone when safer, narrower-spectrum options are available.
A 4-year-old with CAP and concurrent purulent sinusitis, amoxicillin in past 30 days. Best empiric choice?
A. High-dose amoxicillin
B. Amoxicillin–clavulanate
C. Azithromycin
D. Doxycycline
E. Ceftriaxone IM single dose
Compare management of a 3-year-old with suspected viral CAP (mild symptoms) versus a 12-year-old with suspected Mycoplasma pneumoniae. Discuss diagnostic testing thresholds, empiric antibiotic choices (amoxicillin vs macrolide), and when to add antivirals during influenza season.
Q: Do most preschool CAP cases need antibiotics?
A: No. Most are viral; reserve antibiotics for convincing bacterial disease (AAP Red Book 2024).
Q: When should I choose a macrolide?
A: In school-aged/adolescents with clinical features suggesting atypical pathogens (e.g., Mycoplasma).
Q: Should antivirals be started before confirming influenza?
A: Yes, for hospitalized or severe/progressive cases—do not delay pending tests (CDC 2024).
Q: First-line outpatient therapy for typical bacterial CAP in a 3-year-old?
A: High-dose amoxicillin targeting S. pneumoniae.
Find this and other Pediatric Medicine exam prep questions in Med-Challenger Pediatric Medicine Exam Review with CME
Try for free and save. Ace your exams and meet your CME/MOC requirements for just $35 a month!
No matter your program, no matter the size, Med-Challenger for Groups and Institutions can better prepare your program or group, fulfill industry requirements, and increase test scores.
Exam-focused review: distinguish neonatal vascular lesions, cephalohematoma, and caput — high-yield Peds Prep question.
Med-Challenger FUSE is an all new look, with new capabilities, and lots of new features.
Med-Challenger FUSE Joint Commission CME has an all new look, with new capabilities, and lots of new features.
Stay informed of new medical education content, certification requirements and deadlines, case-based CME quizzes, and special offers.