Most Missed Question — Pediatric Emergency Medicine
This week's most‑missed Pediatric Emergency Medicine question with a concise explanation and exam‑focused takeaways for PEM board/in‑training prep.
ABP pediatrics most-missed question with concise explanation and a test-taking tip for board prep.
Key takeaway: For trisomy 18, the primary risk factor across pregnancies is advancing maternal age due to increased meiotic nondisjunction; most cases are not inherited.
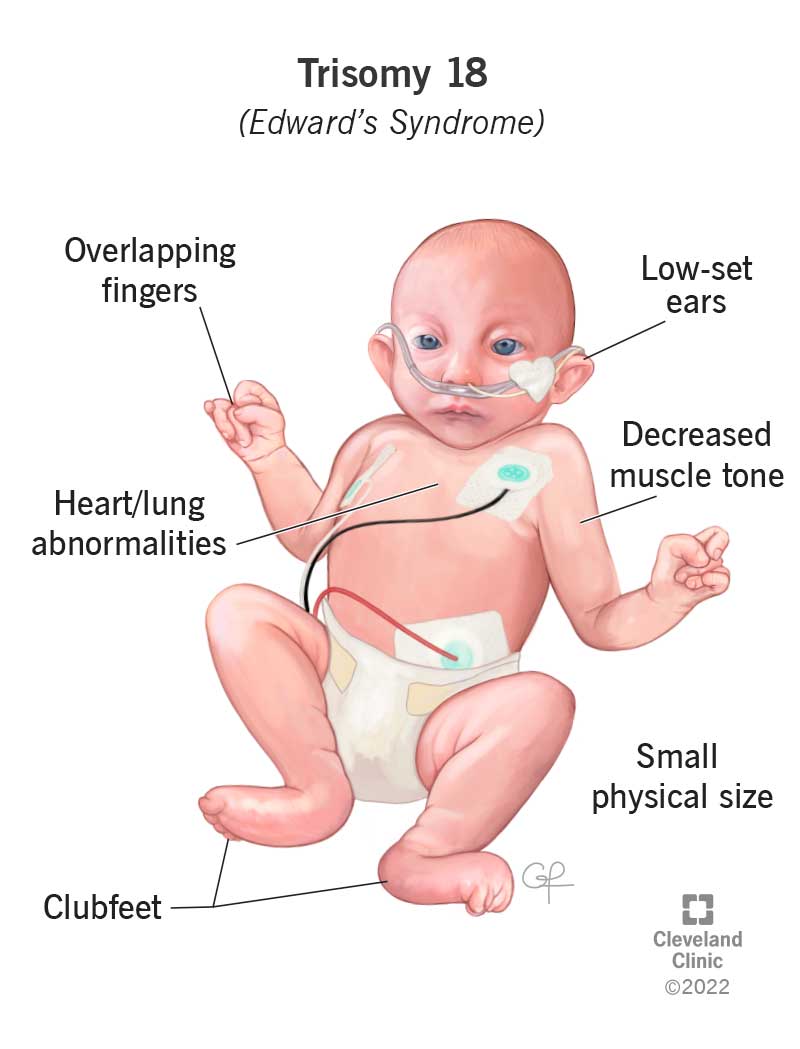
A newborn is born with multiple birth defects. Prenatal complications included oligohydramnios and intrauterine growth retardation. Findings on physical examination are notable for abnormal facies (eg, microphthalmia, orbital hypertelorism, cleft lip), hypotonia, microcephaly, skeletal abnormalities (eg, clenched hands with the index finger overriding the middle finger and the fifth finger overriding the fourth finger), and heart murmur.
You decide to obtain imaging as well. Computed tomography (CT) of the chest is notable for pulmonary hypoplasia. CT of the head indicates holoprosencephaly. Echocardiography is remarkable for a large ventricular septal defect and patent ductus arteriosus. Findings on cytogenetic studies indicate a diagnosis of Edwards syndrome.
What is a risk factor for future pregnancies (ie, giving birth to a child with Edwards syndrome)?
Answer Options:
A. increased maternal age
B. genetic testing indicates trisomy 18
C. genetic testing indicates mosaic trisomy 18
D. oligohydramnios noted during prenatal period
Many test-takers overthink this item because the stem mixes features more classically tied to trisomy 13 (eg, holoprosencephaly, cleft lip) with hallmark Edwards findings (overlapping fingers, growth restriction, VSD), then anchors on cytogenetics confirming trisomy 18. The question asks about future risk—an epidemiology/counseling pivot—so the correct move is to abstract away from the phenotype and recall that the dominant risk factor for trisomy 18 is advancing maternal age via meiotic nondisjunction.
On exams, “is X a risk factor for future pregnancies?” tests understanding that most trisomy 18 cases are sporadic and not inherited. Mosaicism is not a “risk factor,” and oligohydramnios is a consequence, not a cause. When translocation trisomy 18 is suspected, parental karyotyping matters; otherwise, maternal age remains the key risk factor to remember (American College of Obstetricians and Gynecologists [ACOG] Practice Bulletin 226, 2020; Society for Maternal-Fetal Medicine [SMFM] Consult, 2021).
| Option | What It Tests / Implies | Why It’s Wrong Here |
|---|---|---|
| genetic testing indicates trisomy 18 | Confuses diagnosis with risk factor | Confirms the current case, not a predictor for future pregnancies unless translocation; most T18 are sporadic nondisjunction. |
| genetic testing indicates mosaic trisomy 18 | Misinterprets mosaicism as heritable risk | Mosaic T18 typically arises post-zygotically and is not a parental risk factor for recurrence. |
| oligohydramnios noted during prenatal period | Mistakes complications for etiologic risks | Oligohydramnios is a consequence of fetal pathology (eg, growth restriction), not a cause of trisomy. |
Most trisomy 18 cases arise from maternal meiotic nondisjunction; recurrence risk parallels maternal age and is not typically inherited unless a parental balanced translocation is present.
The stem deliberately blends phenotypic features that could suggest trisomy 13 with definitive cytogenetic confirmation of trisomy 18, enticing you to chase phenotype instead of stepping back to answer an epidemiology/counseling question. Boards reward recognizing that “future risk” → maternal age (unless a translocation is identified).
A 36-year-old G2P1 had a prior pregnancy with full trisomy 18 confirmed by karyotype due to nondisjunction. She asks about risk in a future pregnancy. Which factor most strongly influences recurrence risk?
A. Paternal ageSecond-trimester screening shows AFP low, hCG low, unconjugated estriol low, and inhibin A normal. Which diagnosis is most consistent?
A. Neural tube defectA neonate has trisomy 18 due to an unbalanced translocation identified on karyotype. What is the most appropriate next step for recurrence risk assessment?
A. Offer microarray to the neonateWhich neonatal finding most strongly points toward trisomy 18 rather than trisomy 13?
A. HoloprosencephalyA term neonate has multiple anomalies suspicious for trisomy 18. What is the best single confirmatory test?
A. Serum cell-free DNACompare counseling and recurrence risk in two scenarios: (1) a prior pregnancy with full trisomy 18 due to nondisjunction in a 39-year-old, and (2) a neonate with trisomy 18 from an unbalanced translocation with one parent carrying a balanced translocation. How do recommendations for parental karyotyping, preconception counseling, and prenatal diagnostic testing differ?
Yes. ABP/ABIM-style exams and ACOG guidance emphasize that maternal age–related meiotic nondisjunction is the dominant driver of risk for trisomy 18.
Typically no. Mosaicism often arises post-zygotically and is not a parental risk factor; boards expect you to avoid labeling mosaicism as heritable.
When trisomy 18 is due to a translocation on the infant’s karyotype. This materially alters recurrence risk and guides future pregnancy planning.
Low AFP, low hCG, low estriol, with normal (or low) inhibin A—high-yield for exam questions.
Find this and other Pediatric Medicine exam prep questions in Med-Challenger Pediatric Medicine Exam Review with CME
Try for free and save. Ace your exams and meet your CME/MOC requirements for just $35 a month!
No matter your program, no matter the size, Med-Challenger for Groups and Institutions can better prepare your program or group, fulfill industry requirements, and increase test scores.
This week's most‑missed Pediatric Emergency Medicine question with a concise explanation and exam‑focused takeaways for PEM board/in‑training prep.
Most Missed Question in Pediatric Emergency Medicine: concise answer, why it's missed, and a testing tip for PEM exam prep.
Most missed EM exam question: recognizing NAVA (neurally adjusted ventilatory assist) vs time/pressure modes. Quick tips and practice for exam prep.
Stay informed of new medical education content, certification requirements and deadlines, case-based CME quizzes, and special offers.