Question – Cyanotic infant endocarditis
An 8-month-old girl presents with fever, malaise, and 15% weight loss over the past 2 months. She was seen by her pediatrician for an ear infection 1 month ago and treated with amoxicillin. Her mother reports that she improved after that, but today she is getting worse.
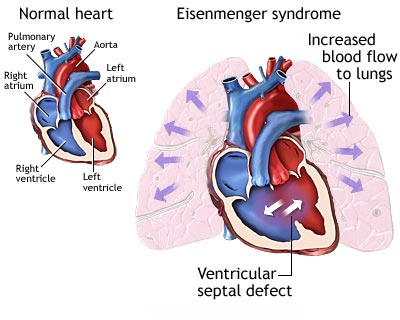
The patient has a history of tetralogy of Fallot. Surgical correction was performed when the child was 6 months of age; residual ventricular septal defect and right outflow obstruction are still present.
The patient’s vital signs are: heart rate 124 beats/minute; blood pressure 75/50 mm Hg; respiratory rate 28 breaths/minute; and temperature 38.8 °C.
On examination, she is cyanotic, and her lungs are clear, but she has a harsh 3/6 systolic murmur. This is consistent with the residual ventricular septal defect.
Which of the following would be the most common pathologic finding in this patient?
Answers:
A. congestive heart failure (CHF)B. secondary valvular heart disease
C. tuberculosis (TB)
D. infective endocarditis (IE)
Correct option: D. infective endocarditis (IE)
This item is missed because the stem’s hemodynamics (tachycardia, hypotension), weight loss, and cyanosis tempt examinees toward CHF or chronic infections like TB. But on the boards, the highest-yield signal is recent repair of congenital heart disease with residual defects in an infant with persistent fever—classic for pediatric infective endocarditis. American Heart Association/American Academy of Pediatrics guidance (2015 statement; reaffirmed in practice via 2021 AHA/ADA prophylaxis update) emphasizes congenital heart disease as the dominant predisposing condition for pediatric IE, with risk heightened in the postoperative period and with residual shunts or prosthetic material.
For exam performance, anchor on epidemiology: in children, congenital heart disease accounts for the majority of IE, and fever is by far the most common presenting symptom. Organisms are most often viridans group streptococci and Staphylococcus aureus. Recognizing this pattern prevents overcalling CHF (a complication, not the “most common pathologic finding”) and avoids distractors like TB.
Why This Question Is Frequently Missed
- “Most common pathologic finding” is interpreted as a complication (CHF) rather than the underlying disease process (IE).
- Weight loss and prolonged fever cue examinees toward TB; the stem’s cardiac risk factors are more determinant on boards.
- Underestimation of postoperative IE risk in infants with residual defects after congenital heart surgery.
What the Distractors Indicate
| Option | What It Tests / Implies | Why It’s Wrong Here |
|---|---|---|
| CHF | Recognizing decompensated heart failure signs | CHF is a possible complication but not the most common pathologic process driving this presentation; fever predominates in pediatric IE. |
| Secondary valvular heart disease | Thinking of rheumatic/degenerative valvular pathology | Unlikely in an 8-month-old; the key risk is CHD with residual VSD/obstruction, not acquired valvular disease. |
| TB | Chronic infection causing fever/weight loss | Epidemiology and risk factors don’t fit; no TB exposures are provided, and cardiac history strongly favors IE. |
| Infective endocarditis | Association of CHD and postoperative period with IE | Correct: CHD (especially with residual defects) is the leading predisposing factor for pediatric IE; fever is the most common symptom. |
High-Yield Pearl
In pediatrics, congenital heart disease—particularly post-repair with residual defects—is the top risk factor for infective endocarditis; expect viridans streptococci and Staphylococcus aureus as the leading pathogens.
Core Learning Objectives
1. Recognize congenital heart disease (and recent repair/residual defects or prosthetic material) as the primary predisposing factor for pediatric infective endocarditis and its typical presentations (fever > any single complication).2. Identify the most common microbiology of pediatric IE and understand timing/context (viridans streptococci with oral sources; Staphylococcus aureus with healthcare exposure/lines; increased risk early post-surgery).
The “Test Trick” at Play
The stem blends nonspecific systemic features (fever, weight loss) with a high-yield risk flag (postoperative CHD with residual VSD). Boards reward pattern recognition: when a child with residual congenital lesions has persistent fever, select infective endocarditis over complications or unrelated chronic infections.
Additional Practice Questions and Remediation for Pediatric Infective Endocarditis
Family Medicine Practice Question 1 - Post-dental fever in repaired VSD
A 7-year-old with a repaired VSD and a small residual shunt develops persistent fever and a new murmur 2 weeks after a dental extraction. Which organism is most likely?
- A. Staphylococcus aureus
- B. Coagulase-negative staphylococci
- C. HACEK organisms
- D. Candida albicans
- E. Viridans group streptococci
Family Medicine Practice Question 2 - Central line toddler with fever
A 2-year-old with short-gut syndrome and a tunneled central venous catheter presents with high-grade fevers and a new murmur. Most likely pathogen?
- A. Enterococcus faecalis
- B. Staphylococcus aureus
- C. Viridans group streptococci
- D. Streptococcus pneumoniae
- E. Bartonella henselae
Family Medicine Practice Question 3 - Early post-repair tetralogy
A 4-year-old boy with a history of tetralogy of Fallot repaired six months ago presents for a routine follow-up visit. His mother reports he tires more easily during play compared to other children. Physical exam reveals a grade 2/6 systolic murmur at the left upper sternal border and a normal S2. Oxygen saturation is 97% on room air.
Which of the following is the most appropriate next step in management?
- A. Begin empiric diuretic therapy for right heart failure
- B. Obtain an echocardiogram to assess for residual right ventricular outflow obstruction and pulmonary regurgitation
- C. Order a chest CT to evaluate for pulmonary artery stenosis
- D. Reassure the mother that mild fatigue is expected after repair
- E. Schedule a cardiac MRI to assess for aortic root dilation
Family Medicine Practice Question 4 - Dental prophylaxis scenario
Which child requires antibiotic prophylaxis for a dental extraction per current recommendations?
- A. Innocent Still’s murmur, otherwise healthy
- B. Completely repaired VSD with no residual defect, >1 year post-repair
- C. Repaired tetralogy with residual VSD jet across a patch
- D. Prior Kawasaki disease without coronary aneurysm
- E. Functional (physiologic) tricuspid regurgitation
Mini Case Discussion Prompt
Compare the likelihood and microbiology of infective endocarditis in: (1) a 9-year-old with native bicuspid aortic valve and recent dental work; (2) a 2-year-old with a tunneled central line; and (3) an 8-month-old 4 weeks post-VSD patch with a residual shunt. How do risk contexts shift the most probable pathogens and urgency of echocardiography/blood culture strategies?
Mini-FAQ
- Do boards expect classic peripheral stigmata (Osler nodes, Janeway lesions) in pediatric IE vignettes? Rarely; ABFM exams more often cue with fever + CHD risk factors and a murmur rather than peripheral signs.
- Which organisms should I think of first in pediatric IE? Viridans group streptococci and Staphylococcus aureus; choose based on exposure (oral/dental vs. healthcare/line).
- How does timing after CHD repair affect risk? Highest within months of surgery, especially with residual defects or prosthetic material; this is a high-yield test clue (AHA/AAP 2015).
- Is CHF the most common presentation? No—fever is. CHF is a complication and less common at initial presentation.
Find this and other Family Medicine exam prep questions in Med-Challenger Family Medicine Review with CME
Try for free and save. Ace your exams and meet your CME/MOC requirements for just $35 a month!
No matter your program, no matter the size, Med-Challenger for Groups and Institutions can better prepare your program or group, fulfill industry requirements, and increase test scores.