What is the Best Family Medicine Question Bank? We Compare ABFM QBanks
What is the best family medicine Qbank for ABFM board review, really? How to choose the best family medicine question bank for ABFM board exam prep.
Most Missed Family Medicine Question — Meningitis vs Endocarditis. Quick answer, key CSF and exam clues for Family Medicine board prep.
Bacterial meningitis — acute fever, nuchal rigidity, AMS and CSF with neutrophilic pleocytosis, low glucose and high protein. Endocarditis is more subacute with new murmur, positive blood cultures and vascular phenomena; on exams prioritize time course and CSF findings.
A 55-year-old man who lives alone is brought in by his neighbors because of severe altered mental status, confusion, and severe headache. They state that he normally seems healthy, but he had recently been "quite sick" with fever. The patient himself is confused, and he cannot provide additional history.
The patient appears acutely ill. He is disoriented to time and place. Vital signs are as follows: heart rate 105 beats/minute and regular; blood pressure 115/60 mm Hg; respiratory rate 16 breaths/minute; and temperature 39.4 °C (103 °F). The lungs are clear. There is a grade III diastolic murmur along the left sternal border. No gallop is detected. In addition to confusion, the neurologic examination reveals mild right-sided motor weakness, more pronounced in the arm than the leg. There is a moderate increase in muscle tone on the right side and reflexes on that side are hyperactive. There is a Babinski sign on the right as well. A careful skin examination does not reveal any lesions. The remainder of the physical examination is normal. Laboratory studies:
CBC reveals normal hemoglobin and hematocrit, normal red blood cell indices, and a modest neutrophilic leukocytosis (WBC 12,000 with 90% neutrophils).
Electrolytes, BUN/Creatinine, serum calcium, liver function studies, and urinalysis are all normal.
Blood cultures are pending.
Computed tomography (CT) of the head is performed and is significant for small aneurysms located at the distal branching points of the left middle cerebral artery.
The diagnostic test that might provide the most useful information pending the results of blood cultures is which of the following?
Answer Options:
A. Magnetic resonance angiography (MRA)
No, it’s not a novel-length reading comprehension test. You could be forgiven for thinking that, but…. 🙂
This is about prioritizing diagnoses by immediacy of threat. The author wants you to pick the next diagnostic step that answers the most life‑threatening possibility first. The vignette mixes signs of infective endocarditis and focal neurologic deficit. That is intentional. It creates a common boards trick where test-takers reach for cardiac tests instead of ruling out acute CNS infection.
| Option | What It Tests / Implies | Why It’s Wrong Here |
|---|---|---|
| Magnetic resonance angiography (MRA) | Evaluates intracranial vasculature and aneurysm anatomy; useful for characterizing mycotic aneurysms. | Useful later, but does not rule out acute meningitis. It delays diagnosis of the most immediately life‑threatening possibility. |
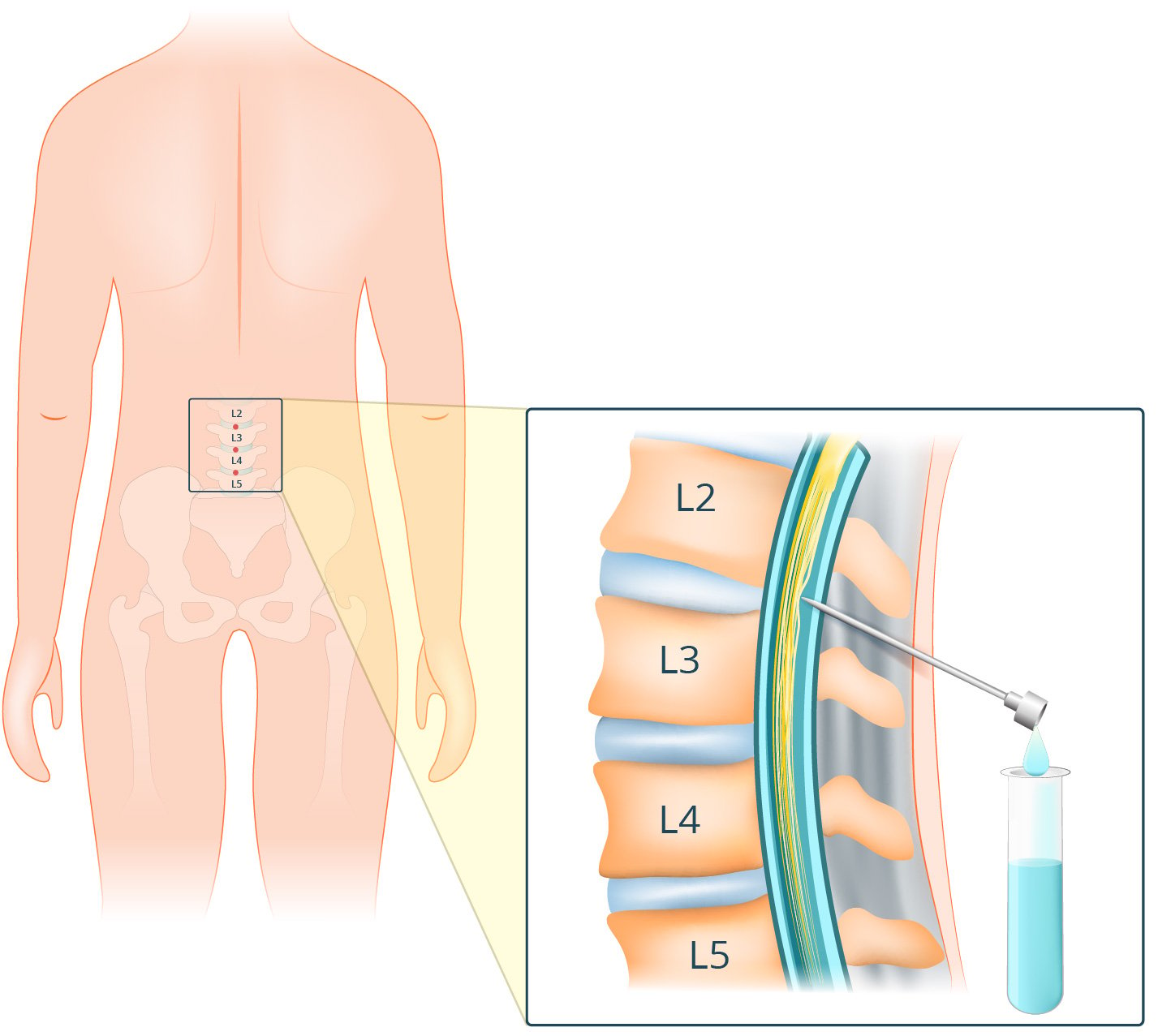
| Lumbar puncture | Tests CSF to confirm or exclude meningitis/central nervous system infection. | Correct — it addresses the highest‑priority, potentially reversible threat in this presentation, provided no contraindication on head imaging. |
| Electrocardiogram (ECG) | Screens for arrhythmia, conduction abnormalities, or ischemia that might complicate cardiac disease. | Low yield for the presenting neurologic febrile syndrome; does not change immediate neurologic management. |
| Echocardiography | Detects valvular vegetations and structural lesions causing endocarditis. | Important for diagnosing endocarditis, but should follow more urgent evaluation for CNS infection when that is a competing life‑threatening diagnosis. |
If bacterial meningitis is on the differential and head imaging shows no mass effect or contraindication, perform lumbar puncture promptly — it addresses the most immediately life‑threatening diagnosis.
This is an order‑of‑operations trap. The vignette deliberately provides findings that support a high‑yield noncardiac emergency (fever, altered mental status) and concurrent findings that suggest a cardiac source (diastolic murmur, mycotic aneurysms). The exam tests whether you choose the diagnostic step that addresses the most time‑sensitive, potentially reversible condition (meningitis) rather than the tempting confirmatory test for the chronic/underlying disease (echo or MRA).
A 62‑year‑old woman presents with 2 days of fever, headache, and progressive confusion. She has a history of prosthetic aortic valve replacement last year. On exam she is febrile (39°C) and somnolent but arousable. Neurologic exam shows left facial weakness and left arm drift. Noncontrast head CT shows no mass effect or hemorrhage. Blood cultures are being drawn. Which test provides the most immediate diagnostic information?
A. Chest x‑ray
B. Carotid duplex ultrasound
C. Transesophageal echocardiography (TEE)
D. Lumbar puncture
E. MRI brain with contrast
A 48‑year‑old man with IV drug use history presents with sudden severe headache, fever, and right‑sided weakness. He is febrile and confused. Noncontrast head CT shows subarachnoid blood in the left sylvian fissure and small distal MCA branch aneurysm. Blood cultures pending. Which test is most important now?
A. Immediate lumbar puncture
B. CT angiography of the head
C. Transthoracic echocardiogram (TTE)
D. Start empiric IV antibiotics without further testing
E. Electroencephalography (EEG)
A 70‑year‑old man with known native aortic valve regurgitation presents with fever and acute expressive aphasia. He is febrile and appears ill. Head CT is normal. Blood cultures are being obtained. Which next step best balances diagnostic urgency and safety?
A. Immediate lumbar puncture prior to antibiotics
B. Start broad‑spectrum antibiotics and defer LP entirely
C. Obtain urgent transthoracic echocardiogram now
D. Do MRI brain to look for ischemic stroke before LP
E. Obtain a lumbar puncture after taking blood cultures and before antibiotics
A 55‑year‑old man is brought in with fever, new right leg weakness, and a new diastolic murmur. He is confused. Noncontrast head CT shows multiple small infarcts in the left MCA territory but no mass lesion. Blood cultures are pending. What test should you do next?
A. Lumbar puncture
B. Magnetic resonance angiography (MRA) of the brain
C. Transesophageal echocardiogram (TEE) after blood cultures
D. Serum cryptococcal antigen
E. Carotid magnetic resonance angiography
A previously healthy 40‑year‑old presents with fever, headache, and new-onset seizures. He is somnolent and febrile. Exam shows a systolic murmur. CT head shows patchy hypodensities consistent with early infarcts; no midline shift. Blood cultures are pending. Next best diagnostic step?
A. Immediate EEG to evaluate seizures
B. Lumbar puncture after CT head and before antibiotics
C. Start IV steroids and wait for cultures
D. CTA head and neck to evaluate for dissection
E. Order urine toxicology screen
Compare and contrast the diagnostic sequencing and immediate management in a febrile patient with focal neurologic deficits when head CT is (a) normal with no mass effect, (b) shows ischemic infarcts only, and (c) shows hemorrhage/SAH — how does each scenario change the prioritization of LP, vascular imaging, echo, and empiric antibiotics?
Find this and other Family Medicine exam prep questions in Med-Challenger Family Medicine Review with CME
Try for free and save. Ace your exams and meet your CME/MOC requirements for just $35 a month!
No matter your program, no matter the size, Med-Challenger for Groups and Institutions can better prepare your program or group, fulfill industry requirements, and increase test scores.
What is the best family medicine Qbank for ABFM board review, really? How to choose the best family medicine question bank for ABFM board exam prep.
How to prepare for your family medicine board exam. ABFM study guide. How to pass the ABFM board exam. ABFM exam tips.
How to prepare for your 2022 family medicine board exam. 2022 ABFM study guide. How to pass the ABFM board exam. ABFM exam tips.
Stay informed of new medical education content, certification requirements and deadlines, case-based CME quizzes, and special offers.